By Sharon S. Shepard

“Did a doctor tell you to do this or is it a personal preference?”
I glared at the snarky nurse over my mask. I had already explained my lymphedema to my doctor, the lab supervisor, and two administrators before entering her clinic. Now this woman implied I was crazy to want blood drawn from the top of my foot, when regular labs aren’t allowed to perform the procedure.
My condition is a mystery to most doctors and nurses because they can’t see it and it’s not well-covered in school – it’s called Stage One Lymphedema, in both arms. When I was diagnosed with bilateral early-stage breast cancer in 2017, the standard of care required removal of up to five sentinel lymph nodes on each side to check them for cancer. My surgeon was careful, and my nodes were all clear, but surgery on the tiny lymphatic vessels can leave scar tissue and blockage.
Fortunately, my hospital provided a lymphedema awareness seminar after surgery. A physical therapist explained the goal of avoiding infection and trauma to the at-risk arms and recommended compression sleeves to prevent lymphedema when flying. Lymphedema can show up years, even decades after damage to the lymphatic system – when an event over-stresses these vessels that drain white blood cells and heavy fluid from tissues.
To prevent trauma and infection, medical procedures like blood draws, IVs, vaccinations, and blood pressure checks should be done on an arm that isn’t at risk for lymphedema, especially during the healing time after surgery. But when I asked about my bilateral situation, the physical therapist shook her head – the recommendation was to alternate arms and hope for the best. Instead, I made a “Sophie’s Choice,” and sacrificed my left arm for medical procedures. I protected my dominant right arm, which had previously been shattered in a car accident.
A mosquito bite launched my lymphedema. The allergic reaction above my left elbow preceded swelling below it. This was not normal swelling – it tingled and ached and burned at night and wouldn’t go away on its own. Ice did not help, and I knew heat would make it worse. After a couple of months, I consulted my oncology massage therapist, who is also certified for lymphedema therapy. She performed manual lymphatic drainage and told me to wear my compression sleeve every day and stop lifting heavy objects – this was the best treatment available in 2018. The swelling and restrictions were a constant reminder of my cancer treatment and made me question its value. But with therapy and time, my left arm swelling is now periodic, and my right arm has only one node that seems to pop up when I fly.
Healthy legs can be used for medical procedures, but unsuspecting nurses threaten my arms with blood pressure cuffs and needles at every doctor’s visit. They’ve never heard of my bilateral situation, so I have to explain it, again. But my arms are worth the surprised expressions, doubtful laughter, and inconveniences. I’ve trained nurses to measure blood pressure at the ankle, gotten vaccines in my thigh, had minor surgeries without IV anesthesia, and made arrangements to have blood drawn from my feet. I’m avoiding trauma and infection in my arms, so my sluggish lymphatic vessels won’t be overwhelmed, especially as I age.
I worry about other cancer survivors who haven’t had my training, so aren’t protecting and watching at-risk limbs. It’s essential to recognize and treat lymphedema in early stages, because damage done by long-term lymphatic swelling is hard to reverse. Many women, including the heroic actress and activist, Kathy Bates, have later stage lymphedema in both arms. More education and research on early-stage lymphedema is needed for patients as well as medical providers so we can prevent later-stage lymphedema.
The good news – we learn more about lymphedema every year, and effective treatments are coming. ICG Lymphography was approved by the FDA in 2018 to scan the lymphatic system, so even early-stage lymphedema can be seen, diagnosed, and studied with something besides a tape measure. Microsurgeons are using ICG Lymphography with improved techniques to re-route blocked lymphatic vessels. Lymphedema research is finally catching up with the progress made in cancer treatment over recent decades.
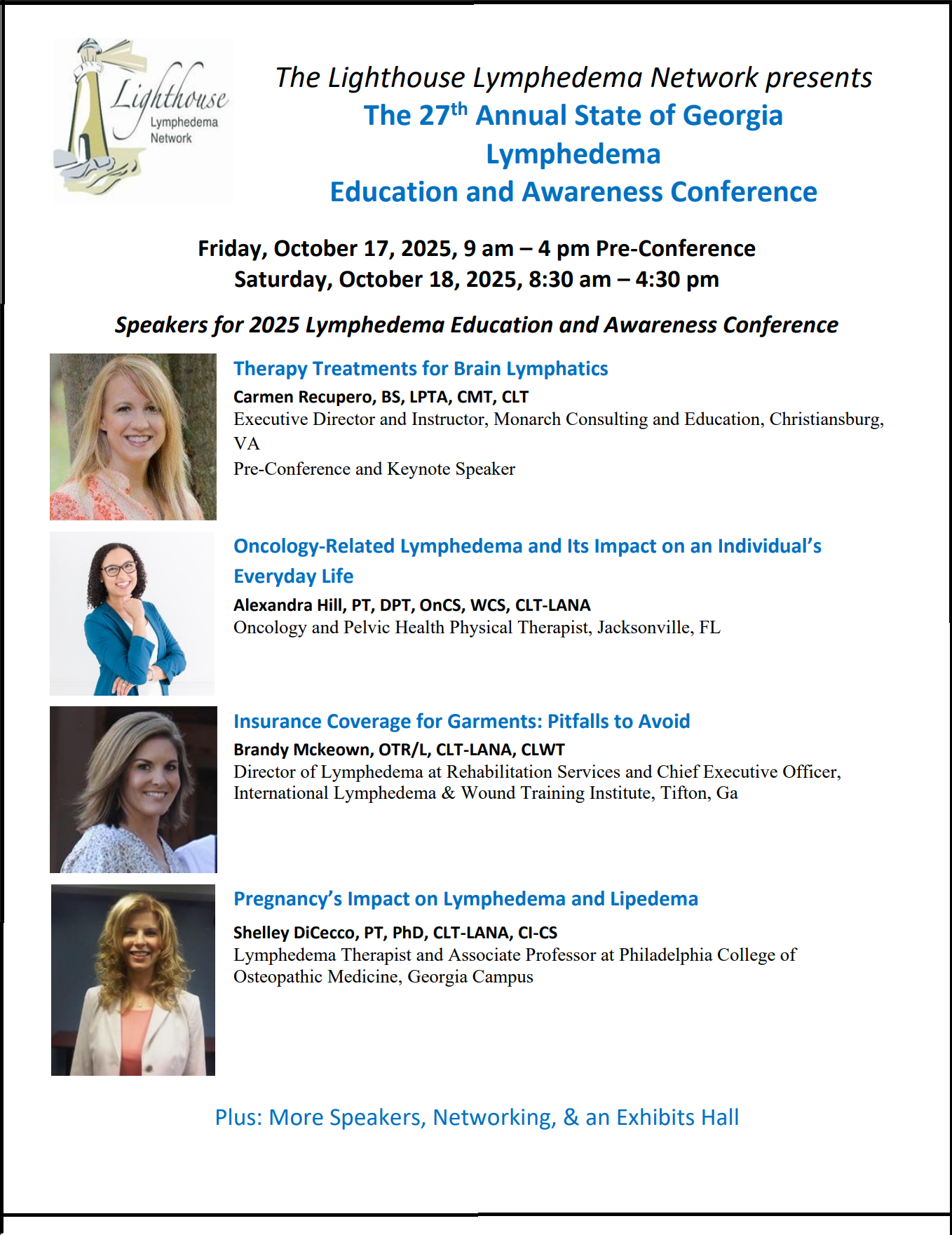
I am grateful to organizations like Kathy Bates’ Lymphedema Education & Research Network and my Atlanta-based Lighthouse Lymphedema Network for their efforts promoting lymphedema awareness, research, and treatment. Their websites and seminars have provided information and encouragement as I’ve struggled with the medical system. And I am not alone – thousands of lymphedema sufferers benefit from the advocacy work of dedicated volunteers, therapists, and researchers solving the mysteries and challenges of lymphedema.



 Welcome To The Lighthouse
Welcome To The Lighthouse